In our previous blog on use cases for AI assistants in healthcare, we looked at where generative AI is already being applied and why adoption in this sector is unique. The next challenge for leaders is proving whether these assistants deliver measurable ROI.
Healthcare organizations are under pressure to justify their AI investments. Unlike traditional systems, the impact of AI assistants is diffuse and often long-term. A triage bot may shorten calls and improve patient experience, but how much of that can be attributed directly to the AI? A scribe might reduce burnout, but the financial benefit may not appear until years later in reduced turnover.
Breaking ROI into three parts
To make ROI concrete, leaders can split it into three connected layers:
Financial returns
Direct savings and revenue impacts, such as fewer denied claims, reduced overtime, or more patients seen per day. AI scribes that save hours each week can quickly add up across a clinical workforce.
Operational efficiency
Improvements like shorter call times, higher completion rates, or fewer readmissions when discharge instructions are clearer. These reduce costs and improve capacity.
Non-financial value
Better patient trust, lower clinician stress, or improved staff retention. These may not show up in this quarter’s balance sheet but are vital to long-term sustainability.
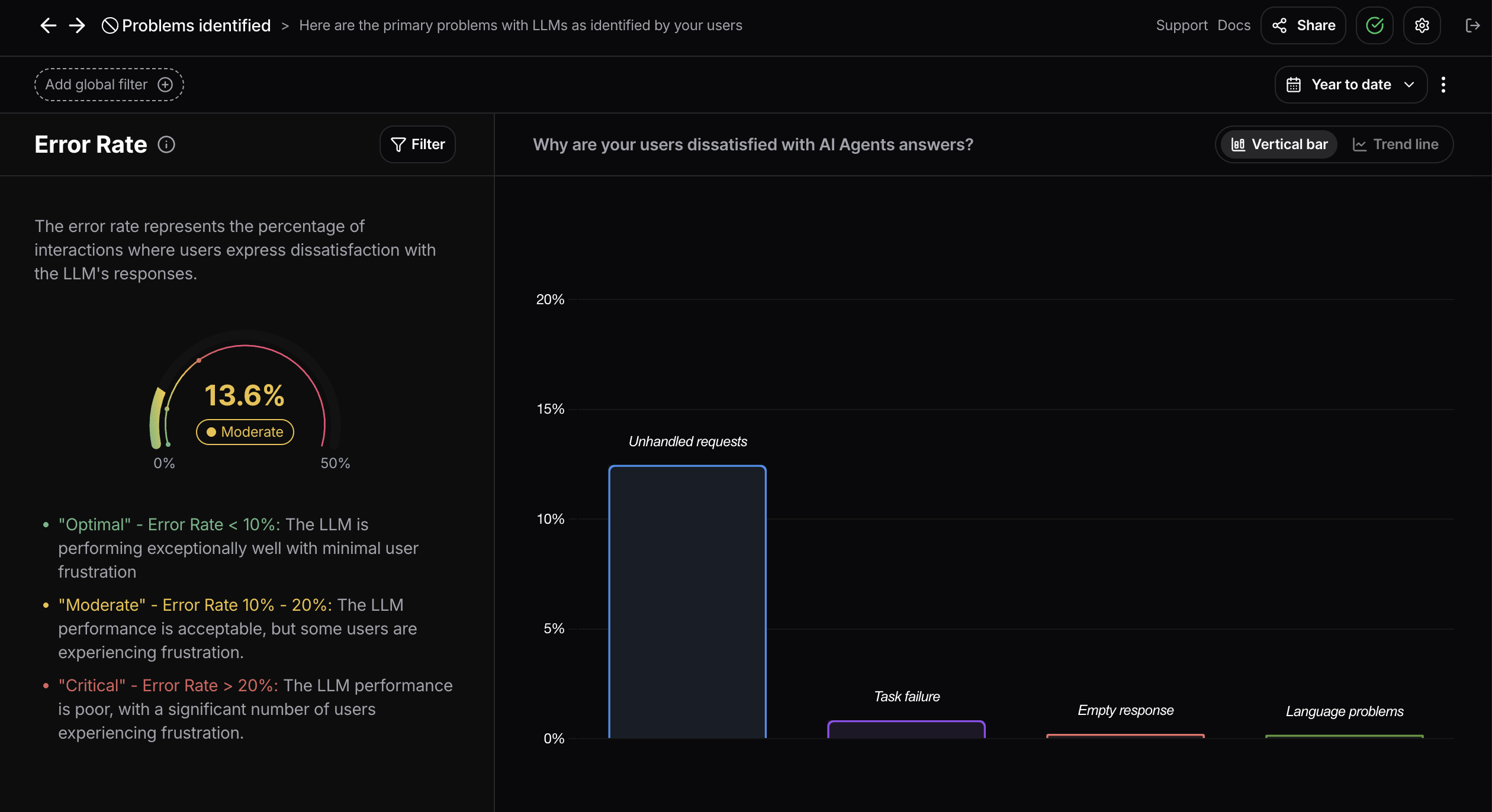
Why technical metrics fall short
System KPIs such as uptime, latency, or token usage are necessary but not sufficient. They show how the system runs, not how people experience it. A chatbot may handle thousands of queries quickly, but if 40% of users drop out mid-session, the ROI is weak.
This is why user analytics is essential. Metrics like topic analysis, retention rate, risky behavior, and error rate provide the missing context. They reveal what people actually do, whether they keep using the assistant, whether unsafe interactions are occurring, and how often humans need to correct outputs.
Four user analytics signals that link to ROI
- Topic analysis shows what tasks dominate usage. If scheduling requests are common but often fail, the weak link is obvious. Aligning investment with high-volume topics prevents wasted effort.
- Retention rate tracks whether clinicians and patients return to the assistant after first use. Sustained retention is the clearest sign of real value; low retention means ROI will not materialize.
- Risky behavior flags unsafe prompts or compliance breaches, such as inclusion of personal health data or inappropriate medical advice requests. Preventing incidents avoids fines, liability, and reputational damage.
- Error rate shows how often outputs fail in real use. An answer may be technically correct but wrong in context, such as applying adult dosage guidelines to a child. These misses force overrides, cancel time savings, and erode trust. Lower error rates mean outputs are not just accurate but safe and usable, which strengthens ROI.
Together, these signals link real behavior to financial and clinical outcomes.
A practical framework for ROI measurement
1. Set baselines before deployment. Capture current times, error rates, and satisfaction scores.
2. Define success metrics upfront. Include financial goals and user analytics: topic analysis, retention rate, risky behavior, and error rate.
3. Instrument assistants for live tracking. Monitor both outcomes and behaviors, not just API calls.
4. Use dashboards to combine signals. For example: hours saved, higher completion rates, improved retention, and fewer risky events.
5. Communicate results in both dollars and care impact. Link savings to staff workload, patient throughput, and safety improvements.
6. Iterate. If retention is low or error rate high, refine prompts, training, or guardrails and re-measure.
Guardrails and trust
ROI depends on safe, trusted assistants. Guardrails are needed to block unsafe advice, monitor for risky behavior, and ensure human oversight where required. Error rate monitoring builds confidence that outputs are reliable. These protections drive adoption, which in turn drives ROI.
Conclusion
Proving ROI for AI assistants in healthcare is not straightforward, but it is achievable. Leaders need to go beyond system logs and measure three layers: financial outcomes, operational efficiency, and user behavior. The most critical signals are topic analysis, retention rate, risky behavior, and error rate.
Healthcare organizations that measure these signals gain both evidence for the boardroom and a feedback loop to improve ROI over time. That means fewer stalled pilots, stronger adoption, and AI tools that truly support clinicians and patients.
If you are deploying AI assistants in healthcare, book a demo with Nebuly to see how user analytics can help you prove and improve ROI.